by Lottie Ayres

Lottie Ayres is a Volunteer Pharmacist on the Drugs in Breastmilk (DiBM) Team at the Breastfeeding Network. She lives in the North East of England and volunteers with her local Maternity and Neonatal Voices Partnership as well as supporting local infant feeding and mental health charities.
Her pharmacy background includes a PhD in Pharmaceutics and Chemistry, some manufacturing and formulation research within the pharmaceutical industry, plenty of Community Pharmacy locum shifts and a brief stint training in a specialist mental health Trust in London. She can now mostly be found running around after two children, identifying plants to forage, and exploring with her two big soppy dogs.
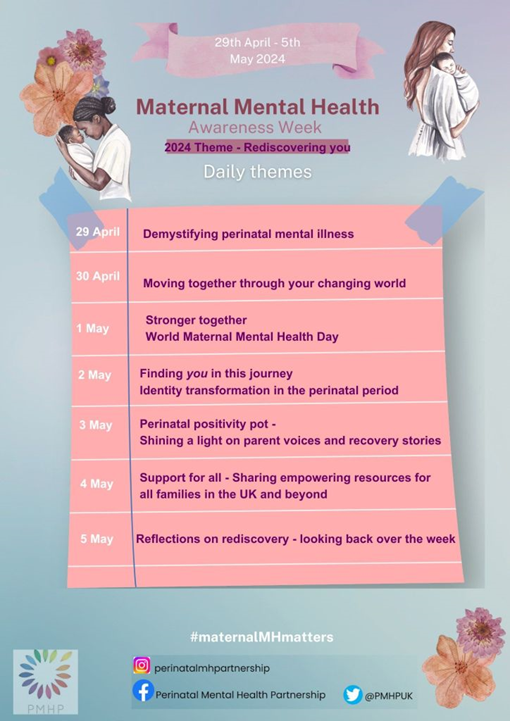
In 2016, the first Wednesday in May became World Maternal Mental Health Day. A year later, the Perinatal Health Partnership UK (PMHP) launched the UK’s first ever Maternal Mental Health Matters Awareness Week. This year the week runs from April 29th – May 5th, with the theme, “Rediscovering You”.
Content Warning
Firstly, I want to share a warning that I will be writing about all things maternal mental health, including mentions of psychosis, trauma and suicide. It is important to me that we talk openly about these things when we can. But sometimes it can feel challenging to read, and sometimes we just aren’t in a place to be able to handle it, and that’s OK. Acknowledging this is important too.
Please know that if you are struggling, there is support available:
- Samaritans – call free anytime – 116 123 or find out more on their website.
- You can also find more local services on the NHS website.
Maternal Mental Health
I offered to write about Maternal Mental Health for so many reasons, from simply wanting to start conversations, and being open about how challenging becoming a parent can be, to acknowledging the huge value in truly listening to another human. I would also like to highlight the gratitude and privilege I feel each time a parent contacts the Drugs in Breastmilk Pharmacy Volunteers to share their feelings or experiences and ask for support.
There is such courage in reaching out when we are finding things hard, and I truly believe that knowing when to ask for help is a superpower (but one that can take a bit of time to learn and retain, certainly from my own personal experience anyway)!
My Pharmacy profession and personal passion for all things maternity mean that I talk about mental health at least once a day, and I am often surrounded by those who appear to be comfortable discussing it (or maybe I just leave them little choice!). I often wonder whether this is truly the case for everyone though. On the surface we certainly seem to be talking about mental health more frequently than when I was growing up. But it’s clear from the heart-breaking statistics that there is still so much more that needs to be done, particularly when it comes to maternal mental health.
The ‘Saving Lives Improving Mothers’ Care 2023’ report tells us that:
- “Suicide continues to be the leading cause of direct maternal death between six weeks and twelve months after birth, accounting for a staggering 39% of deaths in this period”
- “37% of the women who died were known to have a previous or existing mental health condition”
These statistics can sound scary. But if perinatal mental health problems can affect one in five women or birthing people, then we should be talking about it as much as we can even if it feels a bit uncomfortable.
Despite my passion, I struggled to know what to write, so I decided to ask some local mothers and parents about their lived experience of maternal mental health problems, and they kindly shared their key messages.
“Perinatal mental health problems can be experienced by anyone.”
There are risk factors that may increase the likelihood of someone becoming unwell, such as a history of mental health problems or previous traumatic experiences (see Mind’s website for more details). But this is not an exhaustive list. It is possible to become unwell even if you have always experienced good mental health previously.
“Seek out help early”
Seeking Support
Perinatal mental illnesses may range from mild symptoms through to a severe medical emergency, but in all circumstances, it is crucial to seek out specialist support and treatment as soon as possible.
PANDAS have a toolkit that can be downloaded and used as a template for supporting you to have these conversations when visiting your GP / health visitor / midwife or any other healthcare professional you might feel comfortable talking with. It can be found here.
It can also be used as a guide for considering how you’re feeling, whether those emotions have been consistent or getting worse, and whether there might be a need to seek out help. The page suggests keeping track of your mood each day, or even throughout the day if that feels appropriate, and offers a scoring system out of 10 which includes:
0 = I’m feeling hopeless / this is the worst I’ve ever felt
10 = I’m very happy / this is the best mood I’ve ever felt.
The more we raise awareness of what to watch out for, the earlier we will be able to ask for help.
“Know where to find help”
In addition to that superpower of knowing when to ask for help, we also need to know where to go and who to talk to. In many cases, the first port of call would be our midwife, health visitor or GP. But if you are in crisis, it may also be the local A&E, or the Samaritans.
For those who are experiencing severe or complex mental health problems, there are specialist perinatal mental health teams around the UK, which include Community Teams, and Mother and Baby Units (MBUs). You can find more information on Community Perinatal Mental Health Services here.
“Know where to find out more”
There is a wealth of information out there about perinatal mental health problems, which is wonderful thing, but it can also be hugely overwhelming and sometimes a challenge to decipher fact from fiction. The Mind website talks through each of these illnesses in more detail, highlighting symptoms and linking to a range of treatment options.
“Don’t shy away from using the real terms”
The mental illnesses that are often discussed in relation to maternal health are:
- Perinatal depression
- Perinatal anxiety
- Perinatal obsessive-compulsive disorder (OCD)
- Postnatal post-traumatic stress disorder (PTSD) and birth trauma
- Postpartum psychosis
Some people may also experience eating disorders perinatally. There are specialist webpages and charities set up to raise awareness for each of these conditions. I want to mention postpartum psychosis specifically, as it requires specialist treatment urgently. It is a severe but also very treatable condition from which nearly all mums recover fully. Action on Postpartum Psychosis is a national charity that promotes awareness, facilitates research and offers peer support for this illness.
Postpartum Mental Health and Breastfeeding
There is research that highlights many links between postpartum mental health and breastfeeding (or chest feeding), and though the relationship is not clearly understood, we do know that stopping breastfeeding before a mother is ready can result in grief and trauma.
You can find studies that look at the links between breastfeeding and mental well-being in mothers here. Professor Amy Brown also has a collection of resources on supporting breastfeeding grief.
“Seek out support for medication and breastfeeding”
Medication and Breastfeeding
Research tells us that many mothers will choose to postpone their own treatment to continue to feed if they are told they must choose. It is hugely important that parents are enabled to make an informed choice about medication and breastfeeding.
It is often possible to continue breastfeeding whilst taking medication for a mental health condition. Please contact the Drugs in Breastmilk service if you have been told you need to stop breastfeeding in order to take medication, or are thinking about delaying your treatment to keep breastfeeding.
The DiBM service has several factsheets covering topics such as anxiety, depression and OCD. There is also the option to contact the team of Pharmacist Volunteers directly and engage in a conversation through Facebook messenger or email. There are specialist resources we can share and discuss in more detail with you, and we often answer direct queries from healthcare professionals too.
“You can make a full recovery”
Raising Awareness
This is such an important point to highlight, especially after the startling statistics on those experiencing perinatal mental illness. This is not to downplay the challenges people face, but there are so many stories of hope out there from parents who have experienced perinatal illness and recovered in full, as well as those who continue to share their experiences to raise awareness. Please do go and take a look, here.
“The more we talk about it, the better chance we have of making change”
The best way to raise awareness and overcome any stigma we might feel is to keep talking about mental health with as many people as will listen to us. Sharing trusted resources and information with women, birthing people and their families can open up conversations and allow these discussions to become part of our everyday chats. It can be scary, but being honest and sharing when we’re having a challenging day, or week, or month not only gives us the chance to feel heard and understood, but it can give other people the permission they may need to share their feelings too!
My Personal Thoughts
It feels important for me to share a tiny bit about my personal experience of motherhood. The whistle-stop tour is that there has been pregnancy loss, hyperemesis gravidarum and anxiety, as well as an undertaking of kinship care, which opened my eyes to a very different route of becoming a parent.
My conclusion is that becoming a mother is a time of huge changes, whether we are talking about the physical changes occurring within our body to grow and nourish them, or the incomprehensible changes to our professional and social lives, not to mention the many tiny adjustments we make to our world as a whole to incorporate a mini human within it. And this conclusion is not just my own, there is a science to it, and it even has its own term ‘Matrescence’!
Change can feel hugely uncomfortable regardless of how much we want it to happen. There is science behind this too, and I can’t help but feel that if becoming a parent were seen as a job, there would be consultants advising us on each of the stages, supporting us through the cycles of pre-contemplation, contemplation, preparation, action and maintenance!
Yes, we have antenatal classes, hypnobirthing, and parent support groups, however, mostly we just muddle on through by ourselves. That being said, I don’t truly believe that anything could have prepared me fully for the wild ride that is motherhood. Learning to let go of any hint of perfection or control, sharing our vulnerabilities and finding time to care for ourselves amidst the chaos, are very much a work-in-progress for me.
What makes the biggest difference for me is when I’m brave, vulnerable and connected with another human, enabling each of us to see that we don’t have to experience this wild ride alone. For example, this process of sharing a tiny bit of my story right here (terrifying but good, I hope), or helping load shopping for the stressed mother comforting her toddler in front of me in the supermarket queue, or asking for help from a fellow parent because I am having one-of-those days and can picture exactly where on the kitchen table I left the nappies. On the days I’m not feeling so brave, heading out for a walk, connecting with nature, and sharing a smile with a stranger (or if I am being totally honest, usually their dog!) can normally do the trick. But on the days that I just cannot bring myself to leave the house, hunting out my journal and getting the feelings out onto paper can often be a good place to start!
70% of women either hide or underplay the severity of their mental health problems – this statistic really helps to remind me that sharing our challenging moments with others may feel uneasy, but it might just give them the freedom to share theirs too, and there is such healing to be found in offering space for our stories.
Thank you so much for reading!
Lottie
Here are some more places for support and information:
Perinatal Mental Health Partnership
Action on Postpartum Psychosis
NHS Accessing Mental Health Services
Free suicide awareness training
Northern Ireland only, Lifeline – phone 0808 808 8000 or access

