by the DiBM staff team and Emma Thomas
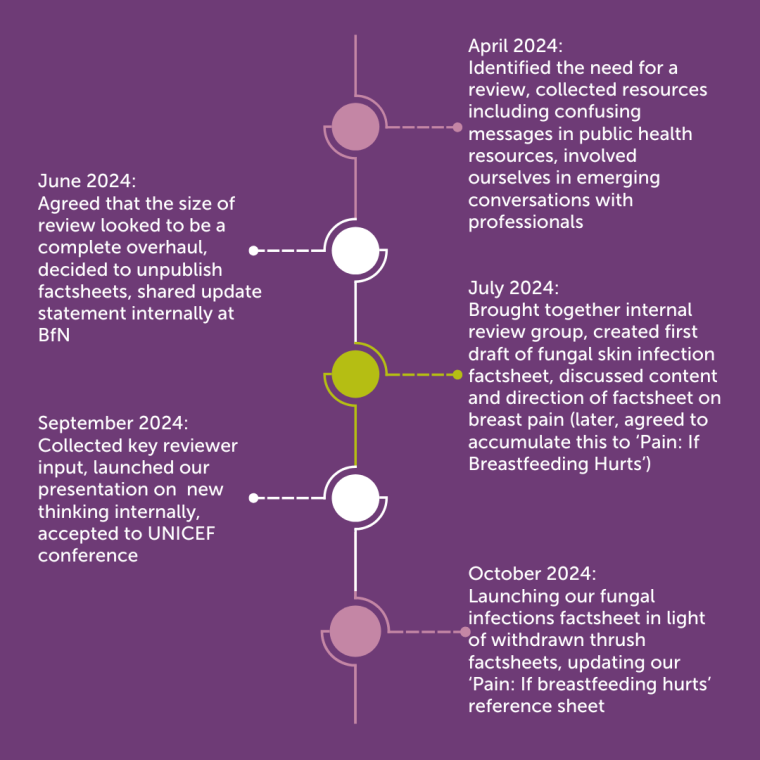
You may have noticed recently that the Drugs in Breastmilk (DiBM) factsheets on thrush of the nipple or breast have been taken down. This is because our clinical pharmacy team have spent the last six months challenging the status quo when it comes to persistent nipple or breast pain whilst breastfeeding. We recognise that anyone who has been treated for breast thrush may have difficult feelings to process at this news.
We took these resources down whilst we considered how best to reorganise our information on breast pain in line with up-to-date guidance, research and best practice. We will not be publishing new factsheets on breast/nipple thrush. Instead, we encourage parents, breastfeeding supporters and healthcare professionals to prioritise skilled breastfeeding support and consider all other possible causes of breast/nipple pain.
It has become common for parents who report persistent breast pain during breastfeeding to be diagnosed with breast or nipple thrush, without all other possible causes of pain being excluded first. With that diagnosis made, the breastfeeding parent and infant are typically prescribed an antifungal medicine to address their symptoms.
Recent research highlights the uncertainty around breast/nipple thrush as a common cause of breast pain. Publications by Betts, Douglas, Jiménez and Plachouri explain that the evidence does not support the diagnosis of breast/nipple thrush as a cause of breast pain. They emphasise that multiple other possible causes of pain should be considered first and that treatment with antifungals is therefore unnecessary and unhelpful. Prescribed and over-the-counter medication are being used in the place of skilled support, without addressing the cause of the problem, causing a premature end to breastfeeding journeys.
In line with guidance from NICE, we are therefore encouraging our colleagues in healthcare and breastfeeding support to challenge the pervasive narrative around thrush in the interests of patient care and medicines optimisation. At BfN, we will move forward by focusing on our superpower: a skilled peer supporter’s ability to support breastfeeding parents experiencing breast or nipple pain.
At DiBM, we will continue give information on medication compatibility with breastfeeding; even where that medicine is to be used following a diagnosis of nipple/breast thrush. But our service’s volunteer pharmacists also have a moral responsibility to challenge the existing thrush narrative, in support of antimicrobial stewardship and to protect breastfeeding.
How can we all support parents with persistent breast/nipple pain whilst breastfeeding?
At BfN, we will continue to support breastfeeding parents experiencing pain according to our core principles and using our expertise, as recommended by NICE guidance. The cornerstone of good breastfeeding support is listening to a parent’s story about their breastfeeding experience, observing a feed from start to finish (where in-person support is possible), and asking what’s changed recently. Ideally, this support would be delivered face-to-face. You can find details of groups where BfN peer supporters offer skilled support here, or ask a midwife or health visitor about services in your area. For those parents who are not able to access face-to-face support or prefer an alternative, our colleagues on the National Breastfeeding Helpline are committed to providing comprehensive remote assistance to parents 24 hours a day, 7 days a week, including thorough support with breastfeeding technique, often referred to as Posture, Positioning, Approach and Attachment.
There won’t be a one-size-fits-all pathway for working though breast pain. Parents will need individualised, person centred care. Our Pain: if breastfeeding hurts page is a good first port of call for anyone experiencing, or supporting someone experiencing, breast pain.
If pain persists despite skilled breastfeeding support, we should look at all possible causes. These should be investigated in a stepwise approach. Infection should only be diagnosed by an appropriately trained and qualified clinician. While our breastfeeding supporters can signpost to a healthcare professional for further investigation, it is out of their remit to diagnose an infection. This highlights the importance of working together as a skilled multidisciplinary team, and we are communicating this work to the healthcare professionals we are in touch with.
We are proud to be publicly sharing the journey we are taking as we examine the evidence and develop our information and practice on this nuanced and evolving topic.
Support available from The Breastfeeding Network
Our National Breastfeeding Helpline volunteers are excellently placed to offer support by phone or social media, whilst our peer supporters at drop-in groups and on postnatal wards can provide support face-to-face. This is the expert support that NICE guidance on managing breastfeeding problems refers to. You can also get in touch if you have questions or are experiencing difficult feelings regarding your own breastfeeding experience after reading this information. Our supporters are here for you.
For any queries relating to taking medication whilst breastfeeding please contact the Drugs in Breastmilk team by email or on their Facebook page. Please note, the team is comprised of volunteers, who prioritise responding to medication-related questions from parents. If you have a general question related to the withdrawal of our factsheets on breast thrush that does not require an urgent response, you can contact admin@breastfeedingnetwork.org.uk.
Acknowledgements
Particular thanks is extended from the Drugs in Breastmilk Service to Dr Naomi Dow, for engaging in an ongoing conversation with the team about leading this shift within our services.

