This information can also be viewed as a PDF by clicking here.
This factsheet is intended to provide access to relevant evidence-based information. The national guidelines, research, data, pharmacokinetic properties and links shared are taken from various reference sources, they were checked at the time of publication for appropriateness and were in date. These are provided where we believe the information may be useful but we do not take any responsibility for their content. This factsheet is provided to empower users to make an informed decision about their treatment; but it does not constitute medical advice and cannot replace medical assessment, diagnosis, treatment or follow up from appropriately trained healthcare professionals with relevant competence.
The Breastfeeding Network factsheets will be reviewed on an ongoing basis, usually within three years or sooner where major clinical updates or evidence are published. No responsibility can be taken by the Breastfeeding Network or contributing authors for the way in which the information is used.
If you have any questions about this information, you can contact the Drugs in Breastmilk team through their Facebook page or on druginformation@breastfeedingnetwork.org.uk.
There is little research on the safety of dental treatment during breastfeeding but many mothers undertake treatments without harm on a daily basis. The risk of interrupting breastfeeding and substitution of formula appears greater (Dorea 2004).
Fillings
There is no reason to avoid inserting or replacing fillings during breastfeeding. One report suggests that it is prudent to avoid unnecessary removal of fillings during pregnancy or lactation (Barreguard 1995). However there are occasions when a new mother may need a filling inserted or replaced. When mercury is removed some will be vaporised by the high-speed drill and a very small amount may be swallowed or inhaled. These amounts are minute and passage into breastmilk is insignificant compared to the background levels of mercury in the environment. The limitation of the consumption of tuna in line with the FSA guidance is more important on limiting the body burden of mercury and it is very difficult to prove any link between mercury fillings and long term health problems (Lawson). Preventative dental health to minimise the risk of decay is perhaps the message which is of paramount importance.
White fillings
In some parts of the UK white fillings are recommended in pregnancy and lactation following an EU Directive (July 2018) but have to be paid for by the patient rather than being part of free NHS treatment. The information states that “These restrictions on the use of dental amalgam aim to help reduce environmental mercury pollution and are not a result of any safety concerns about amalgam fillings for dental patients.”
“According to the new regulations, the use of dental amalgam is no longer allowed for the treatment of children under 15 years old or of pregnant or breastfeeding women, unless the dentist thinks that it is necessary. These restrictions on the use of dental amalgam aim to help reduce environmental mercury pollution and are not a result of any safety concerns about amalgam fillings for dental patients. If you are pregnant or breastfeeding, the new regulations apply to you. This means that, to reduce dental amalgam use, your dentist will not usually use dental amalgam to fill your teeth while you are pregnant or breastfeeding.”
“If you need a filling when pregnant or breastfeeding, there are materials other than dental amalgam that your dentist can use.” https://www.sdcep.org.uk/published-guidance/dental-amalgam/
Local anaesthetic
There is no evidence to interrupt breastfeeding after the use of local anaesthetics. Local anaesthetics work by deadening sensation of the nerve endings around the tooth. There is no evidence of passage into breastmilk and therefore no reason not to continue breastfeeding. The addition of adrenaline to the anaesthetic to reduce bleeding may possibly make a sensitive baby jumpy and irritable so it may be worth asking the dentist to limit use if possible.
For more information, see our factsheet on local anaesthetics whilst breastfeeding.
Tooth extraction
There is no evidence to interrupt breastfeeding after tooth extraction. If a tooth is to be removed the mother is likely to be offered a local anaesthetic injection or sedation. She may also need pain killers and/or antibiotics.
Sedation/general anaesthetic
You can breastfeed after a general anaesthetic or sedation as soon as you are awake and alert. However, you may feel drowsy, and your judgement may be impaired for up to 24 hours afterwards, so you will need to have another adult with you who can look after you and help you care for your child. For more information, see our factsheets on dental sedation and anaesthetics.
Analgesics (pain killers)
Breastfeeding mothers may take paracetamol and/or ibuprofen in normal doses after dental treatment. See our factsheet on analgesics for more information.
Antibiotics
Breastfeeding mothers may take antibiotics in normal doses after dental treatment and continue to breastfeed. Babies may have looser bowel motions and may be windy. See our factsheet on antibiotics for more information.
Other dental agents
- Mouthwashes – can be used by a breastfeeding mother as they will not be absorbed into the bloodstream e.g. Corsodyl®, Chlorhexidine mouthwash, Difflam®, Benzydamine mouthwash
- Gels and liquids for mouth ulcers e.g. Anbesol®, Bonjela®, Medijel®, Rinstead®, Iglu®, Orajel® can all be used
- Fluoride toothpastes can be used during breastfeeding. Although there is no research the absorption from the teeth would be minimal and swallowing of excess is unlikely, e.g. Durophat®
Tooth whitening
There appears to be no information available on the use of tooth whitening agents during lactation. Whilst it is unlikely that any significant transfer of the agents used into breastmilk will take place, it is unlikely that urgent treatment is necessary and can be delayed until breastfeeding has finished naturally. Unless the products spill from the bath in which the liquid is placed, absorption is unlikely.
Breastfeeding and Dental Health of the Baby
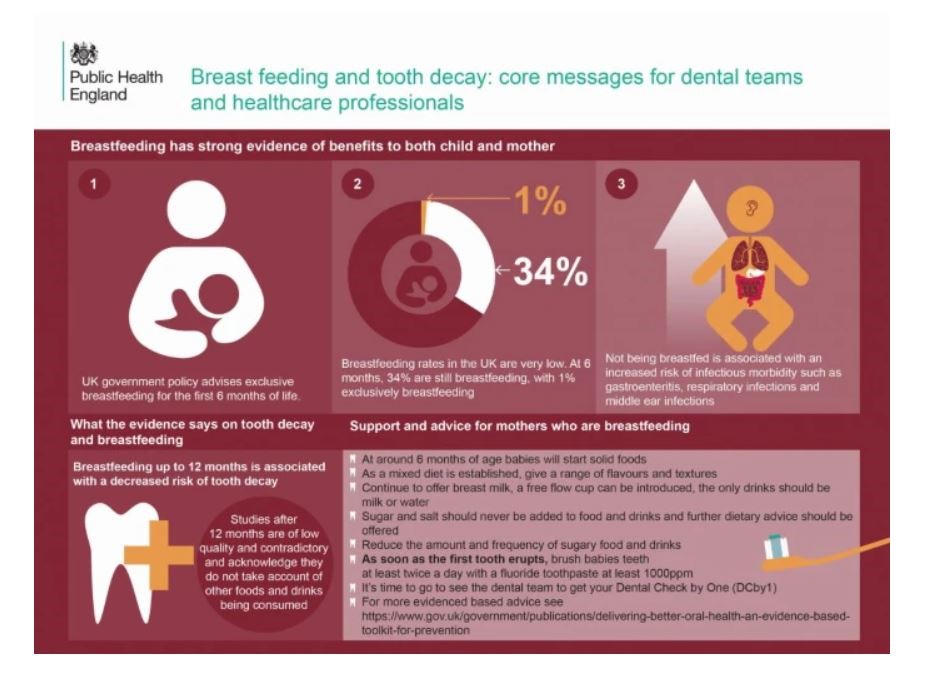
- BDA Breastfeeding – what are the benefits?: Food Fact Sheet https://www.bda.uk.com/resource/breastfeeding.html
- PHE Breastfeeding and dental health https://www.gov.uk/government/publications/breastfeeding-and-dental-health/breastfeeding-and-dental-health
- New advice issued on breastfeeding and dental decay. Br Dent J226, 248 (2019).
- Public Health England. ‘Delivering Better Oral Health: An Evidence-Based Toolkit for Prevention’ 2014 (viewed on 3 August 2018)
- Public Health England. ‘Health Matters: Child Oral Health’ 2017 (viewed on 19 September 2018)
- Tham R and others. ‘Breastfeeding and the risk of dental caries: a systematic review and meta‐analysis’ Acta Paediatrica 2015: volume 104(S467):62-84
- Peres K and others. ‘Breastfeeding and Oral Health: Evidence and Methodological Challenges’ Journal of Dental Research 2018: volume 97(3): 251-8
- Peres K and others. ‘Impact of Prolonged Breastfeeding on Dental Caries: A Population-Based Birth Cohort Study’ Pediatrics 2017: volume 140(1): 2016-2943,
References
- Barreguard et al 1995 Occupational and Environmental Medicines
- Dorea JG. Mercury and lead during breast-feeding. Br J Nutr. 2004 Jul;92(1):21-40
- Grandjean et al. Cognitive Deficit in 7 year old children and prenatal mercury exposure 1997 Neurotoxicol Teratol. 1997 Nov-Dec;19(6):417-28 1997
- Peter Lawson BDS, FDS, FRCPS Amalgam and mercury.
CPD (Continued Professional Development) for dentists
For dentists who wish to update their own CPD options around breastfeeding and drugs in breastmilk please see:
- Breastfeeding and Medication: https://breastfeeding-and-medication.co.uk/fact-sheet/breastfeeding-and-dental-health
- The Breastfeeding Network: Supporting Infant Feeding in Your Practice course
©The Breastfeeding Network. Last full review August 2022. Last updated July 2024.

