This information about coronavirus and breastfeeding is checked regularly and will develop in response to guidelines and evidence. This page was last updated on 26th September 2023.
BfN’s Statement on COVID-19 Vaccines while breastfeeding
This statement aims to address the questions we are receiving. It is for information only and not intended to promote the vaccine or replace advice from a healthcare professional.
If you are breastfeeding or giving your expressed milk, you can have any of the vaccines currently available in the UK as long as you meet the other conditions for receiving the vaccine, as set out by the Medicines and Healthcare products Regulatory Agency (MHRA) and Joint Committee on Vaccination and Immunisation (JCVI). You can continue to breastfeed as normal after vaccination.
Statement from the UK Government, dated 10/01/23, checked on 25/09/23:
The JCVI has recommended that the vaccines can be received whilst breastfeeding. This is in line with recommendations from the WHO and countries like the US and Australia. Vaccinated women produce antibodies which help protect them against COVID-19 disease. These antibodies are also found in breast milk and may help protect breast fed babies. Minute traces of vaccine have been found in the breast milk of some vaccinated women but they disappear after a few days. There is no evidence of harm to the baby and any traces are expected to be broken down with breast milk in the baby’s stomach.
FAQs – COVID-19, Vaccines and Breastfeeding, including information on the latest research
Yes. Current evidence suggests that it is safe to breastfeed and continue to offer breastmilk if you have COVID-19, whatever the age of your baby or child. No evidence has been found for COVID-19 being passed through breastmilk. [1, 2, 3, 4]
The World Health Organisation (WHO) states: “mothers with suspected or confirmed COVID-19 should be encouraged to initiate or continue to breastfeed. Mothers should be counselled that the benefits of breastfeeding substantially outweigh the potential risks for transmission.
Mother and infant should be enabled to remain together while rooming-in throughout the day and night and to practice skin-to-skin contact, including kangaroo mother care, especially immediately after birth and during establishment of breastfeeding, whether they or their infants have suspected or confirmed COVID-19.” [5]
In fact, breastmilk is the best source of nutrition for infants and provides protection against many illnesses. If you have confirmed COVID-19 or have symptoms you should take all reasonable precautions to avoid spreading the virus to your baby, including washing your hands before touching your baby, sterilising any breast pump or bottles and washing your hands after changing their nappy.
Consider wearing a face covering or fluid-resistant face mask while feeding or caring for your baby.
If your baby is older it may be safer to leave your mask off to avoid them pulling at it and touching your secretions.
Babies should not wear a face covering or mask as they may risk suffocation.
Multiple research studies have looked at whether the virus can be transmitted though breastmilk, and no evidence has been found for this. Some studies have found fragments of viral RNA in a small number of breastmilk samples, but this is not the same as live virus that could cause an infection. These fragments may also have got into the milk by cross-contamination [3]. No studies have found live virus that could cause a COVID-19 infection in breastmilk samples [1, 2, 3, 4].
One study checked that this was not because the breastmilk samples used for research had been frozen. They found that when live virus was put into a breastmilk sample, the virus was able to survive being frozen and thawed multiple times. This showed that the absence of live virus in breastmilk samples from COVID-19 positive mothers was not because the virus had been killed by freezing. [3]
It is possible that a COVID-19 positive mother could pass the virus to her baby though contact or droplets from her breath. However, research has shown that even when babies stay in close contact with a COVID-19 positive mother, they are unlikely to catch the virus if the mother observes simple infection control measures, such as handwashing and mask wearing. One research study followed 61 COVID-19 positive mothers and their 62 babies for 20 days after birth. The mothers all observed good hygiene and wore a surgical mask whilst breastfeeding or caring for their baby (within 2m of them). 95% of the babies were breastfed. Only one of the 62 babies tested positive for COVID-19 during the study period [6]. Another study looking at 18 COVID-19 positive mothers found viral RNA on a skin swab from a mother’s breast, but this was taken before she washed her breast. Swabs taken after washing did not contain viral RNA that could cause infection [2].
Breastfeeding, and remaining in close contact with their mother, were known to be protective for a baby’s health, even before the pandemic. The research suggests the risks of not breastfeeding and of separating a mother and baby from each other are greater than the risk of keeping them together, even if the mother is positive for COVID-19. Research also suggests that breastmilk from a mother who has tested positive for COVID-19 might actually protect her baby or child from infection. See the FAQ “Can my breastmilk protect my baby from COVID-19?” for more information.
If you are feeling unwell, you can take paracetamol safely whilst breastfeeding. See the FAQ “Can I take medicines for COVID-19 symptoms while I am breastfeeding?” for more information.
If you are too unwell to breastfeed you may still be able to express milk for your baby. Pump equipment and bottles need to be sterilised according to manufacturer’s instructions. Standard milk storage guidelines apply.
It can be difficult to differentiate between a cold, flu and coronavirus. The information in this diagram may help: https://www.bbc.co.uk/news/health-54145299
[1] Peng, S., Zhu, H., Yang, L., et al. (2020). A study of breastfeeding practices, SARS-CoV-2 and its antibodies in the breast milk of mothers confirmed with COVID-19. The Lancet regional health. Western Pacific, 4, 100045. https://doi.org/10.1016/j.lanwpc.2020.100045
[2] Pace, R. M., Williams, J. E., Järvinen, K. M., et al. (2021). Characterization of SARS-CoV-2 RNA, Antibodies, and Neutralizing Capacity in Milk Produced by Women with COVID-19. mBio, 12(1), e03192-20. https://doi.org/10.1128/mBio.03192-20
[3] Krogstad, P., Contreras, D., Ng, H., et al. (2022). No infectious SARS-CoV-2 in breast milk from a cohort of 110 lactating women. Pediatric research, 10.1038/s41390-021-01902-y. Advance online publication. https://doi.org/10.1038/s41390-021-01902-y
[4] Pietrasanta, C., Artieri, G., Ronchi, A., et al. (2022). SARS-CoV-2 infection and neonates: Evidence-based data after 18 months of the pandemic. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology, 33 Suppl 27, 96–98. https://doi.org/10.1111/pai.13643
[5] https://www.who.int/news-room/commentaries/detail/breastfeeding-and-covid-19
[6] Ronchi A, Pietrasanta C, Zavattoni M, et al. Evaluation of Rooming-in Practice for Neonates Born to Mothers With Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Italy. JAMA Pediatr. 2021;175(3):260-266. https://doi.org/10.1001/jamapediatrics.2020.5086
If you are feeling unwell and think you may have coronavirus, you can continue to feed and care for your baby as usual, if you are able to (see FAQ “Can I breastfeed if I have COVID-19?“). You should consider additional hygiene measures to avoid passing the infection to your baby.
The main points include:
- Wash your hands before touching your baby, breast pump or bottles
- Try to avoid coughing or sneezing on your baby while feeding, whether breastfeeding or giving a bottle.*
- Consider wearing a face mask while breastfeeding, bottle feeding or caring for your baby. If your baby is older it may be safer to leave your mask off to avoid them pulling at it and touching your secretions. Discuss options with your midwife, health visitor or GP.
- Follow manufacturers recommendations for pump cleaning after each use.
- If you are feeling too unwell to breastfeed directly consider asking someone who is well to feed your expressed breast milk to your baby.
- If you choose to feed your baby with formula or expressed milk, it is important that you follow the sterilisation guidelines https://www.nhs.uk/conditions/pregnancy-and-baby/sterilising-bottles/ (link checked 26/04/22).
- If you are expressing breast milk in hospital, a dedicated breast pump should be used. The hospital may have guidance about bringing the bottles into the neonatal unit
*This is to ensure good respiratory hygiene when close to your baby such as when feeding, or changing their nappy.
If you are feeling unwell, and have symptoms of coronavirus, the general information provided in these links should be helpful.
The NHS has information on what to do if you have coronavirus symptoms here: https://www.nhs.uk/conditions/coronavirus-covid-19/ (checked 31.08.22)
England: https://www.gov.uk/guidance/people-with-symptoms-of-a-respiratory-infection-including-covid-19 (checked 30.08.22)
Wales: https://gov.wales/coronavirus (checked 31.08.22)
Scotland: https://www.gov.scot/coronavirus-covid-19/ (checked 31.08.22)
Northern Ireland: https://www.nidirect.gov.uk/campaigns/coronavirus-covid-19 (checked 31.08.22)
See FAQ “Can I take medicines for COVID-19 symptoms while I am breastfeeding?” for information on medicines that can be taken safely whilst breastfeeding.
If you would like to know more about donor milk as an option while you are ill follow this link to find your nearest milk bank. Supplies are limited, they will do what they can. http://www.ukamb.org/
You can take paracetamol and Ibuprofen safely whilst breastfeeding. For more information on pain relief which may also help to relieve temperature and aches & pains: https://www.breastfeedingnetwork.org.uk/analgesics/
For information on cough and cold remedies when you are breastfeeding see: https://www.breastfeedingnetwork.org.uk/cold-remedies/
For information on products which help to relieve sore throats: https://www.breastfeedingnetwork.org.uk/sore-throats/
For factsheets and information on other medicines, see our Drugs in Breastmilk (DiBM) page, or contact our DiBM team via our Facebook page or via email.
Should you be diagnosed with COVID-19 and be admitted to hospital you may be prescribed stronger medication including anti-virals, see https://www.liebertpub.com/doi/full/10.1089/bfm.2020.0268?fbclid=IwAR2OAUf0u5yEbACcrAydssi7JTS68ZVbHrkOnmQgmYVOrLapM1vvbjYLSmo_source=ETOC&utm_medium=email&utm_campaign=bfm (checked 30.08.22)
Yes. The COVID-19 vaccine is recommended for pregnant women [1, 2] and research has now overwhelmingly shown that COVID-19 vaccination during pregnancy is safe and effective at protecting against severe disease [3, 4, 5]. Pregnant women are at increased risk of serious illness as a result of COVID-19 [6] and the JCVI has placed them in priority group 6, alongside adults under 65 with long term health conditions. The JCVI and RCOG recommend that you have the Moderna or Pfizer/BioNTech vaccines as these have been studied more extensively in the USA [6]. However, if you have already had one dose of the AstraZeneca vaccine you will be encouraged to have the second dose of the same vaccine as there is no evidence of risk nor of benefit in mixing the vaccines. For more information, see Pregnant women urged to come forward for COVID-19 vaccination – GOV.UK (www.gov.uk) (updated 16.12.21, checked 30.08.22).
This text is taken from Coronavirus vaccine – weekly summary of Yellow Card reporting – GOV.UK (www.gov.uk), updated on 4th August 2022:
“The number of Yellow Card reports for pregnant women are low in relation to the number of pregnant women who have received COVID-19 vaccines to date (more than 118,000 women in England have given birth up to end of February 2022 after receiving at least 1 dose of COVID-19 vaccine during or shortly before pregnancy and more than 40,000 women in Scotland and Wales have received at least 1 dose whilst pregnant up to end of March 2022). Pregnant women have reported similar suspected reactions to the vaccines as people who are not pregnant. Reports of miscarriage and stillbirth are also low in comparison to how commonly these events occurred in the UK outside of the pandemic. A few reports of commonly occurring congenital anomalies and obstetric events have also been received. There is no pattern from the reports to suggest that any of the COVID-19 vaccines used in the UK, or any reactions to these vaccines, increase the risk of miscarriage, stillbirths, congenital anomalies or birth complications.”
Vaccination during pregnancy may also give your baby some protection against COVID-19. See the FAQ “Can vaccination in pregnancy protect my baby?” below for more information.
[1] https://www.gov.uk/government/publications/covid-19-vaccination-women-of-childbearing-age-currently-pregnant-planning-a-pregnancy-or-breastfeeding/covid-19-vaccination-a-guide-for-women-of-childbearing-age-pregnant-planning-a-pregnancy-or-breastfeeding#:~:text=COVID%2D19%20vaccination%20is%20strongly,protect%20you%20and%20your%20baby . (Updated 11.04.22, checked 30.08.22)
[2] https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/pregnancy-breastfeeding-fertility-and-coronavirus-covid-19-vaccination/ Updated 22.07.22, checked 30.08.22
[3] Kharbanda EO, et al. Spontaneous abortion following COVID-19 vaccination during pregnancy. JAMA. doi:10.1001/jama.2021.15494
[4] Magnus, MC et al. Covid-19 Vaccination during Pregnancy and First-Trimester Miscarriage N En[gl J Med 2021; 385:2008-2010 DOI: 10.1056/NEJMc2114466
[5] Stock SJ, et al SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland Nature Medicine 2022 https://www.nature.com/articles/s41591-021-01666-2.
[6] Pietrasanta, C., Artieri, G., Ronchi, A., et al. (2022). SARS-CoV-2 infection and neonates: Evidence-based data after 18 months of the pandemic. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology, 33 Suppl 27, 96–98. https://doi.org/10.1111/pai.13643
[7] Mahase E. Covid-19: Pregnant women should be offered Pfizer or Moderna vaccine, says UK advisory committee BMJ 2021; 373 :n1013 https://doi.org/10.1136/bmj.n1013
Yes. There is no evidence that vaccination in pregnancy or before initiation of breastfeeding has any negative impacts on breastfeeding or for the breastfed child. The JCVI and NHS recommend having the vaccine and any boosters as soon as you are offered them, regardless of pregnancy or breastfeeding status [1,2].
Pregnant women are at increased risk of serious illness as a result of COVID-19 and the JCVI has placed them in priority group 6, alongside adults under 65 with long term health conditions. Pregnant women can have any of the three licensed vaccines straight away or at any point during their pregnancy and breastfeed as normal when their baby is born. In pregnancy you will normally be offered the Moderna or Pfizer/BioNTech vaccines. They are both compatible with breastfeeding.
Vaccination during pregnancy may give your baby some protection against COVID-19. Antibodies to COVID-19 have also been found in the breastmilk of vaccinated mothers, which may give their baby some protection against COVID-19. See the FAQs “Can vaccination in pregnancy protect my baby?” and “Can my breastmilk protect my baby from COVID-19?” below for more information.
[1] https://www.gov.uk/government/publications/covid-19-vaccination-women-of-childbearing-age-currently-pregnant-planning-a-pregnancy-or-breastfeeding/covid-19-vaccination-a-guide-for-women-of-childbearing-age-pregnant-planning-a-pregnancy-or-breastfeeding#:~:text=COVID%2D19%20vaccination%20is%20strongly,protect%20you%20and%20your%20baby . (Updated 11.04.22, checked 30.08.22)
[2] https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/pregnancy-breastfeeding-fertility-and-coronavirus-covid-19-vaccination/ Updated 22.07.22, checked 30.08.22
Research has shown that vaccination in pregnancy can provide your baby with antibodies against COVID-19. A number of studies have found COVID-19 antibodies in the umbilical cord blood of babies born to mothers vaccinated in pregnancy, meaning that the vaccination may protect the child from infection once they are born, as well as protecting the mother [1, 2, 3]. These antibodies are also found in the umbilical cord blood of babies born to mothers who were infected with COVID-19 during pregnancy [4]. However, research following babies up for up to six months after birth found that antibodies in babies were at higher levels, and more long lasting, after mothers had been vaccinated in pregnancy, compared to infection in pregnancy. This suggests that maternal vaccination is more protective for babies than maternal infection, and that is it worth getting vaccinated, even if you have had a prior infection [5].
Another study from the centre for disease control in the USA showed that babies born to mothers who were vaccinated during pregnancy were significantly less likely to be hospitalised for COVID-19 in the first six months of life than babies born to non-vaccinated mothers, providing some evidence that vaccination in pregnancy may be protective for new-born babies. [6]
[1] Paul, G., & Chad, R. (2021). Newborn antibodies to SARS-CoV-2 detected in cord blood after maternal vaccination – a case report. BMC pediatrics, 21(1), 138. https://doi.org/10.1186/s12887-021-02618-y
[2] Mehaffey, J. H., Arnold, M., Huffstetler, E., et al. (2021). Successful vertical transmission of SARS-CoV-2 antibodies after maternal vaccination. Birth (Berkeley, Calif.), 48(4), 451–452. https://doi.org/10.1111/birt.12582
[3] Gray, K. J., Bordt, E. A., Atyeo, C., et al. (2021). Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. American journal of obstetrics and gynecology, 225(3), 303.e1–303.e17. https://doi.org/10.1016/j.ajog.2021.03.023
[4] Pietrasanta, C., Artieri, G., Ronchi, A., et al. (2022). SARS-CoV-2 infection and neonates: Evidence-based data after 18 months of the pandemic. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology, 33 Suppl 27, 96–98. https://doi.org/10.1111/pai.13643
[5] Shook, L. L., Atyeo, C. G., Yonker, L. M., et al. (2022). Durability of Anti-Spike Antibodies in Infants After Maternal COVID-19 Vaccination or Natural Infection. JAMA, 327(11), 1087–1089. https://doi.org/10.1001/jama.2022.1206
[6] Halasa, N. B., Olson, S. M., Staat, M. A., et al. Overcoming COVID-19 Network (2022). Effectiveness of Maternal Vaccination with mRNA COVID-19 Vaccine During Pregnancy Against COVID-19-Associated Hospitalization in Infants Aged <6 Months – 17 States, July 2021-January 2022. MMWR. Morbidity and mortality weekly report, 71(7), 264–270. https://doi.org/10.15585/mmwr.mm7107e3
Yes, The JCVI and NHS recommend that the vaccines can be received whilst breastfeeding. This is in line with recommendations from the US and the World Health Organization. [1, 2]
You can have any of the licensed vaccines, as initial doses or as a booster, and continue to breastfeed as normal.
The MHRA states:
“There is no current evidence that COVID-19 vaccination while breastfeeding causes any harm to breastfed children or affects the ability to breastfeed.
COVID-19 vaccines do not contain live components and there is no known risk associated with being given a non-live vaccine whilst breastfeeding. The current advice of the Joint Committee on Vaccination and Immunisation (JCVI) is that breastfeeding parents may be offered any suitable COVID-19 vaccine depending on their age.” [3]
Research has shown that vaccination in breastfeeding mothers has minimal side effects and could be protective for the breastfed infant. See FAQs “Do the vaccines have any side effects that affect breastfeeding, or breastfed children?” and “Can my breastmilk protect my baby from COVID-19?” for more details.
Six research studies have looked into whether vaccine mRNA gets into breastmilk after vaccination [4, 5, 6, 7, 8, 9]. Four of these studies [6, 7, 8, 9] found very small traces of vaccine mRNA in breastmilk from some donors. These mRNA fragments do not appear to be active [9].
[1] https://www.gov.uk/government/publications/covid-19-vaccination-women-of-childbearing-age-currently-pregnant-planning-a-pregnancy-or-breastfeeding/covid-19-vaccination-a-guide-for-women-of-childbearing-age-pregnant-planning-a-pregnancy-or-breastfeeding#:~:text=COVID%2D19%20vaccination%20is%20strongly,protect%20you%20and%20your%20baby . (Updated 10.01.23, checked 25.09.23)
[2] https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/pregnancy-breastfeeding-fertility-and-coronavirus-covid-19-vaccination/ (Updated 24.10.22, checked 25.09.23)
[3] Coronavirus vaccine – weekly summary of Yellow Card reporting – GOV.UK (www.gov.uk) (Updated 08.03.23, checked 25.09.23)
[4] Golan Y, Prahl M, Cassidy A, et al. Evaluation of Messenger RNA From COVID-19 BTN162b2 and mRNA-1273 Vaccines in Human Milk. JAMA Pediatr. 2021;175(10):1069-1071. doi:10.1001/jamapediatrics.2021.1929
[5] https://www.medrxiv.org/content/10.1101/2021.05.23.21257686v1
[6] Yeo KT, Chia WN, Tan CW, et al. Neutralizing Activity and SARS-CoV-2 Vaccine mRNA Persistence in Serum and Breastmilk After BNT162b2 Vaccination in Lactating Women. Front Immunol. 2022;12:783975. Published 2022 Jan 11. doi:10.3389/fimmu.2021.783975
[7] Yeo KT, Chia WN, Tan CW, et al. Neutralizing Activity and SARS-CoV-2 Vaccine mRNA Persistence in Serum and Breastmilk After BNT162b2 Vaccination in Lactating Women. Front Immunol. 2022;12:783975. Published 2022 Jan 11. doi:10.3389/fimmu.2021.783975
[8] Hanna N, Heffes-Doon A, Lin X, et al. Detection of Messenger RNA COVID-19 Vaccines in Human Breast Milk. JAMA Pediatr. 2022;176(12):1268–1270. doi:10.1001/jamapediatrics.2022.3581
[9] Hanna N, De Mejia CM, Heffes-Doon A, et al. Biodistribution of mRNA COVID-19 vaccines in human breast milk [published online ahead of print, 2023 Sep 19]. EBioMedicine. 2023;96:104800. doi:10.1016/j.ebiom.2023.104800
This text is taken from Coronavirus vaccine – weekly summary of Yellow Card reporting – GOV.UK (www.gov.uk), updated on 4th August 2022:
“The MHRA closely monitors the safety of COVID-19 vaccines during breastfeeding, including evaluation of Yellow Card reports for COVID-19 vaccines from breastfeeding women. These reports have been reviewed by the independent experts of the CHM’s COVID-19 Vaccines Benefit Risk Expert Working Group, by paediatric and breastfeeding experts.
There is no current evidence that COVID-19 vaccination while breastfeeding causes any harm to breastfed children or affects the ability to breastfeed.
COVID-19 vaccines do not contain live components and there is no known risk associated with being given a non-live vaccine whilst breastfeeding. The current advice of the Joint Committee on Vaccination and Immunisation (JCVI) is that breastfeeding parents may be offered any suitable COVID-19 vaccine depending on their age.
We have received about 4,000 Yellow Card reports from women breastfeeding at the time of vaccination. Most of these women reported only suspected reactions in themselves which were similar to reports for the general population, with no effects reported on their milk supply or in their breastfed children.
A small number of women have reported decreases in their milk supply, most of which were transient, or possible reactions in their breastfed child. A number of factors can affect milk supply and infant behaviour, including general maternal health, amount of sleep, and anxiety. The symptoms reported for the children (high temperature, rash, diarrhoea, vomiting and general irritability) are common conditions in children of this age, so some of the effects reported may have occurred by coincidence.
The product information for COVID-19 Vaccine Pfizer/BioNTech and COVID-19 Vaccine Moderna has been updated to reflect that the available data are reassuring on safety and that the vaccines can be used during breastfeeding.
A small number of women may experience a reduction in their breast milk production and it may be helpful for breastfeeding women to know how to maintain their breast milk supply, particularly if they are feeling unwell. The NHS website has a good resource for this.”
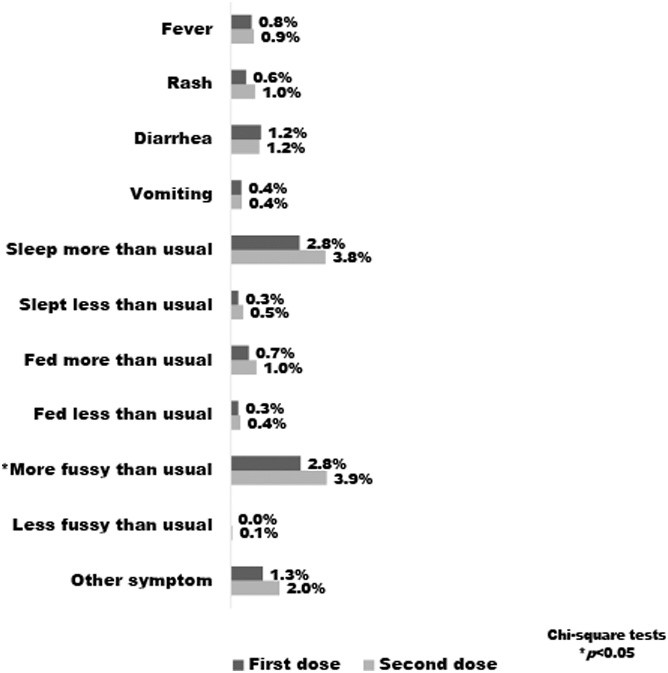
One research study [1] looked at side effects on 4,455 breastfeeding mothers who received either the Pfizer or Moderna COVID-19 vaccination, and their breastfed children. Of these, 77 mothers (1.7%) reported negative effects on breastfeeding. It was noted that these mothers also reported more severe reactions to the vaccine themselves. Overall, 7.1% of mothers reported any symptoms in their breastfed children following COVID-19 vaccination. These were generally mild and are shown in the table below. Other perceived symptoms in the children reported by three or more mothers included runny nose and flushing of cheeks.
The team concluded that COVID-19 vaccination among breastfeeding mothers resulted in minimal impact on breastfeeding and minimal side effects in the breastfed child.
[1] McLaurin-Jiang, S., Garner, C. D., Krutsch, K., & Hale, T. W. (2021). Maternal and Child Symptoms Following COVID-19 Vaccination Among Breastfeeding Mothers. Breastfeeding medicine: the official journal of the Academy of Breastfeeding Medicine, 16(9), 702–709. https://doi.org/10.1089/bfm.2021.0079, https://www.infantrisk.com/content/results-breastfeeding-and-covid-19-vaccine-survey (checked 30.08.22)
Some people report headaches, flu-like symptoms, general aches and pains, nausea, and gastrointestinal symptoms [1]. Taking paracetamol and drinking plenty of fluids to keep you hydrated may help alleviate symptoms. Paracetamol can be taken as normal when pregnant or breastfeeding. See our Drugs in Breastmilk factsheets for more details and information on taking other medicines whilst breastfeeding or the FAQ “Can I take medicines for COVID-19 symptoms while I am breastfeeding?”
As some people report feeling tired in the day or two after the vaccine, you might want to have your vaccine when someone is around to help you care for your baby and bring them to you for feeding. If you usually express milk, you could express some extra ahead of time in case you want to use it. Remember that missing feeds may lower your supply and could lead to blocked ducts or mastitis.
If you believe you have experienced an adverse reaction to a vaccine, you can report this via the yellow card system: https://coronavirus-yellowcard.mhra.gov.uk/ (checked 31.08.22)
[1] Coronavirus vaccine – weekly summary of Yellow Card reporting – GOV.UK (www.gov.uk) (Updated 04.08.22, checked 30.08.22)
Breastmilk from mothers who have been infected with COVID-19 has been shown to contain antibodies to COVID-19 [1, 2]. These antibodies are created by the mother’s body in response to infection or vaccination. They may act like a “non-stick coating” [3] in a breastfed child’s mouth, throat and digestive system and give them some protection against infection. Research has shown that these antibodies are able to neutralise the virus, making it unable to cause an infection [1].
Antibodies to COVID-19 have been found in the breastmilk of mothers who have been vaccinated against COVID-19. Research has found that antibodies are consistently present in the breastmilk of vaccinated mothers, but not unvaccinated mothers who have never been infected [4, 5]. These antibodies have been observed as soon as 7 days after the first vaccine dose [6] and for up to 6 months after vaccination [7].
These antibodies have also been found in the saliva [2] and stools [8] of breastfed infants of vaccinated mothers. This shows that they are present throughout the digestive tract of these infants, where they may be providing protection against infection.
Antibodies in breastmilk could still have benefits for older breastfed children, as well as babies. Higher levels of antibodies have been found in the breastmilk of mothers who were breastfeeding children aged over 2 years. [9] This research confirmed the results of previous studies, showing that breastmilk from mothers who have had two doses of the COVID-19 vaccination have SARS-CoV-2 antibodies in their breastmilk two weeks after receiving the second vaccination. These antibodies were not found in mothers who have not been vaccinated. They also found that there were higher levels of antibodies in the milk from mothers who had been breastfeeding for two years or more. This shows that breastmilk could still have important protective benefits for older breastfeeding children, as well as babies.
There is also evidence that breastmilk is generally protective against respiratory illnesses [10]. One observational study looking at children aged 14 and under who attended the emergency room on specific days over a three-month period found that those who had ever been breastfed (even years before the start of the pandemic) were significantly less likely to test positive for COVID-19 than those who had never been breastfed. Whilst there are other factors that could contribute to this effect (variables such as household income were not factored in), this result suggests that breastfeeding could give some long–term resilience to infections that the child may encounter in the future, including COVID-19. [11]
[1] Pace, R. M., Williams, J. E., Järvinen, K. M., et al. (2021). Characterization of SARS-CoV-2 RNA, Antibodies, and Neutralizing Capacity in Milk Produced by Women with COVID-19. mBio, 12(1), e03192-20. https://doi.org/10.1128/mBio.03192-20
[2] Conti, M. G., Terreri, S., Piano Mortari, E. et al. (2021). Immune Response of Neonates Born to Mothers Infected With SARS-CoV-2. JAMA network open, 4(11), e2132563. https://doi.org/10.1001/jamanetworkopen.2021.32563
[3] Can breastfeeding mothers pass on vaccine immunity to their babies? | Evening Standard checked 30.08.22
[4] Perl, S. H., Uzan-Yulzari, A., Klainer, H. et al. (2021). SARS-CoV-2-Specific Antibodies in Breast Milk After COVID-19 Vaccination of Breastfeeding Women. JAMA, 325(19), 2013–2014. https://doi.org/10.1001/jama.2021.5782
[5] Jakuszko, K. et al. Immune Response to Vaccination against COVID-19 in Breastfeeding Health Workers. Vaccines, 2021, 9, 663. https://www.mdpi.com/2076-393X/9/6/663/htm
[6] Baird, J. K., Jensen, S. M., Urba, W. J. et al. (2021). SARS-CoV-2 Antibodies Detected in Mother’s Milk Post-Vaccination. Journal of human lactation : official journal of International Lactation Consultant Association, 37(3), 492–498. https://doi.org/10.1177/08903344211030168
[7] Perez, S. E., Luna Centeno, L. D., Cheng, W. A. et al. (2022). Human Milk SARS-CoV-2 Antibodies up to 6 Months After Vaccination. Pediatrics, 149(2), e2021054260. https://doi.org/10.1542/peds.2021-054260
[8] Narayanaswamy, V., Pentecost, B. T., Schoen, C. N. et al. (2022). Neutralizing Antibodies and Cytokines in Breast Milk After Coronavirus Disease 2019 (COVID-19) mRNA Vaccination. Obstetrics and gynecology, 139(2), 181–191. https://doi.org/10.1097/AOG.0000000000004661
[9] Ramírez DSR, Pérez MML, Pérez MC, et al. (2021). SARS-CoV-2 antibodies in breast milk after vaccination. Pediatrics 148(5). https://doi.org/10.1542/peds.2021-052286
[10] Duijts, L., Ramadhani, M.K. and Moll, H.A. (2009), Breastfeeding protects against infectious diseases during infancy in industrialized countries. A systematic review. Maternal & Child Nutrition, 5: 199-210. https://doi.org/10.1111/j.1740-8709.2008.00176.x
[11] Verd, S., Ramakers, J., Vinuela, I. et al. Does breastfeeding protect children from COVID-19? An observational study from pediatric services in Majorca, Spain. Int Breastfeed J 16, 83 (2021). https://doi.org/10.1186/s13006-021-00430-z
If you are breastfeeding, you can have any of the licenced vaccines offered in the UK. The Pfizer and Moderna vaccines are recommended for people aged under 40 and pregnant women [1, 2]. Children aged under 18 will only be offered the Pfizer/BioNTech vaccine [1].
One study has found that the SARS-CoV-2–specific IgA antibodies (which could provide breastfed infants with protection against COVID-19) were present more frequently in breastmilk after vaccination with the Pfizer or Moderna mRNA-based vaccines, compared with the Astra-Zeneca and Johnson & Johnson/Janssen vector-based vaccine. After the second dose, almost all participants who had the Pfizer or Moderna mRNA-based vaccines had this type of antibody in their breastmilk, compared to less than half of those who had two doses of Astra-Zeneca vaccine, or the single dose Johnson & Johnson/Janssen vaccine.
Additionally, a second type of antibody, IgG, was present in all participants after receiving two vaccine doses, independent of vaccine type. The researchers suggest that an mRNA-based vaccine may be the optimal choice for lactating women when they want to transfer antibodies to their infants. However, all vaccines provide protection against COVID-19 for the mother and result in some antibodies in breastmilk for most women. [3]
[1] https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine/ (updated 21.07.22, checked 30.08.22)
[2] Mahase E. Covid-19: Pregnant women should be offered Pfizer or Moderna vaccine, says UK advisory committee BMJ 2021; 373 :n1013 https://doi.org/10.1136/bmj.n1013
[3] Juncker, H. G., Mulleners, S. J., Coenen, E. et al.(2022). Comparing Human Milk Antibody Response After 4 Different Vaccines for COVID-19. JAMA pediatrics, e220084. Advance online publication. https://doi.org/10.1001/jamapediatrics.2022.0084
Vaccination is recommended during pregnancy and breastfeeding so you can have the jab, including boosters, as soon as you are invited. Vaccination during pregnancy may protect your baby from COVID-19 after birth, and vaccination whilst breastfeeding may provide passive antibody protection to your nursling via your breastmilk. See sections above on “Can vaccination in pregnancy protect my baby?” and “Can my breastmilk protect my baby from COVID-19?” for more information.
Restarting breastfeeding is possible. You can find more information on relactation here in this leaflet from the Association of Breastfeeding Mothers. If you want to re-stimulate your milk supply or talk through your experience, then you can contact the National Breastfeeding Helpline. Our aim is to support individual, informed decisions based on the best data we have.
Informal milk sharing is not recommended, particularly while coronavirus – COVID-19 is such a concern. Although the virus has not been detected in breastmilk, it can stay on the surface of containers and can also be passed on through close contact without the person being aware they have any of the symptoms.
For more information on sharing breastmilk, see:
https://ukamb.org/ukamb-statement-on-breastmilk-sharing/ (checked 31.08.22)
https://europeanmilkbanking.com/joint-emba-and-hmbana-statement-on-milk-sharing-has-been-released/ (checked 31.08.22)
Pasteurised donor milk may be obtained from a milk bank. This remains safe during the COVID-19 pandemic. There is no evidence that COVID-19 is transmitted through breastmilk [1]. Milk banks use rigorous screening, hygiene measures and pasteurisation to ensure the safety of the milk they supply [2]. Pasteurisation has been shown to leave intact protective antibodies to COVID-19 that may be present in the milk [3].
Priority is given to the sickest, most premature babies. Mothers with their own breastfeeding challenges may be able to get donor breastmilk if there are sufficient supplies. For more information, see
https://ukamb.org/ (checked 31.08.22)
https://heartsmilkbank.org/ (checked 31.08.22)
[1] Pietrasanta, C., Artieri, G., Ronchi, A., et al. (2022). SARS-CoV-2 infection and neonates: Evidence-based data after 18 months of the pandemic. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology, 33 Suppl 27, 96–98. https://doi.org/10.1111/pai.13643
[2] https://heartsmilkbank.org/faqs/ (checked 31.08.22)
[3] Perez, S. E., Luna Centeno, L. D., Cheng, W. A. et al. (2022). Human Milk SARS-CoV-2 Antibodies up to 6 Months After Vaccination. Pediatrics, 149(2), e2021054260. https://doi.org/10.1542/peds.2021-054260
If your baby needs to be cared for in a Neonatal Unit (NICU) these links have general information and specific details about COVID-19.
Specific guidance can be seen on the British Association of Perinatal Medicine website, here: https://www.bapm.org/pages/182-perinatal-covid-19-resources (checked 31.08.22). It includes a document called “frequently asked questions within neonatal services” (last updated 13/01/22). This is detailed and written for clinicians.
The section “How do we manage provision of expressed breast milk (EBM) in the NNU when mother is SARS-Co-V positive?” states:
- To date viral RNA has been reported only very rarely in fresh breast milk of COVID-19 confirmed mothers. The database is, however, small. The main risk of breastfeeding for the infant is the close contact with the mother, who is likely to share infective airborne droplets. National advice for well babies of COVID-19 suspected or confirmed mothers is that the benefits of breast feeding outweigh any theoretical risks.
- For unwell or preterm babies in the NNU the evidence is less clear.
- Practitioners should discuss with parents the pros and cons of provision of EBM to babies in the NNU, noting the current uncertainty. A joint decision should be informed by factors including the gestation and clinical condition of the baby, transfer of protective maternal antibodies, the availability of donor breast milk and parental choice. Other coronaviruses are destroyed by pasteurisation.
- SARS-CoV-2 positive mothers who are expressing milk must be facilitated to practise excellent hand hygiene, and care taken to ensure that bottles containing EBM are not externally contaminated. The virus is deactivated by chlorine disinfectants. EBM of COVID-19 suspected or positive mothers should be stored in a separate fridge or freezer from that of non- suspected or negative mothers. NNUs should have clear guidelines around handling, storage and use of EBM in these circumstances and suspected/infected mothers should have exclusive use of a breast pump.
- If it is decided to withhold mother’s own breast milk, the mother should be encouraged to express and discard her milk, to maintain lactation until she is no longer considered infectious (10 days after onset of symptoms). Repeat testing of mother is not necessary. Parents should be signposted to appropriate feeding and emotional support during this period and reassured that breastfeeding can still take place after a period of using donor breast milk / formula if lactation is maintained.
- Consider testing a sample of EBM for SARS-CoV-2 once lactation is established as this may help with future understanding of this virus.
- Lactation is not a contra-indication to COVID-19 vaccination and breastfeeding mothers should be advised to continue breastfeeding after receiving vaccine.
Bliss has a detailed statement covering the care of babies in neonatal units during the pandemic, including what to do if a mother has symptoms of COVID-19 or tests positive. (Statement updated 22.04.22, link accessed 31.08.22). This statement may be of help when discussing the care of your baby with staff on a neonatal unit.
BAPM guidance states that ‘’it is essential that the mother and her partner are never considered to be visitors within the neonatal unit – they are partners in their baby’s care and their presence should be encouraged and facilitated as much as possible.’’ The guidance also stresses the importance of parents being present together, unless this is clearly detrimental to other babies or staff, and that mothers and their babies should be considered ‘the same biological entity’. Their guidance also notes that parental involvement in the delivery of basic tasks and their baby’s care may prove beneficial to units where there are staffing pressures.
The Bliss statement explains that parents who have tested positive for COVID-19 may not be able to access the neonatal unit until they have completed self-isolation, but this should be discussed with the individual neonatal unit. Some units may have solutions to this, particularly in the case of end of life care, when every effort should be made to facilitate parental presence.
If you want to talk through any worries you have related to breastfeeding and COVID- then you can contact the National Breastfeeding Helpline. Trained volunteers will be able to offer you information and support. You can also talk to your midwife, health visitor or doctor.
If your concern is linked to the vaccine or other medications, you can contact our Drugs in Breastmilk team, where trained volunteer pharmacists will be able to discuss your questions or worried with you.
There are a number of other organisations offering support to breastfeeding mothers, and many support groups are running again now. Details of peer support offered by The Breastfeeding Network can be found here. Information on other organisations offering support can be found here
Feeling anxious is a very normal emotion. We have all felt anxious during the coronavirus pandemic. You may have been isolated from your family, or found the usual support was not available. That’s without the extra worry of coronavirus. These feelings are normal yet may feel overwhelming at times. Coronavirus, or COVID-19 feels threatening, both to ourselves and the people we care about. Recognising this threat can help you work out how best to keep yourself safe. Think about what is helping you and what is making you feel worse and then try to protect yourself from the negative things – including restricting time on social media. It is only necessary to seek help if you find your feelings spiralling out of control. Tell your loved ones how you feel, this may be an opportunity to express your frustration and worries, which may be all that you need for just now. You can call the National Breastfeeding Helpline to talk about your concerns related to breastfeeding. If you can feel more confident about how you feed your baby it can take a lot of weight off your mind.
Sources of help:
- One You https://www.nhs.uk/oneyou/every-mind-matters/(Checked 09.23)
- Lots of good information here plus links to online CBT modules here: https://www.breastfeedingnetwork.org.uk/anxiety/(Checked 09.23)
- Mental Health Foundation have published a very good guide here https://mentalhealth.org.uk/coronavirus/staying-at-home(Checked 09.23)
- BfN’s Big Tea Break – Moment of Calm https://www.youtube.com/watch?v=9T3KRiO2kaE– everyday should include at least 5 minutes of calm! (Checked 09.23)
- Anxiety UK have resources specific to coronavirus https://www.anxietyuk.org.uk/blog/health-and-other-forms-of-anxiety-and-coronavirus/ (Checked 25.09.23)
- Headspace has a section on stress and anxiety which may help you ground yourself by listening to your breathing, e.g. https://www.headspace.com/meditation/anxiety(Checked 09.23)
- https://www.mind.org.uk/information-support/coronavirus-and-your-wellbeing/#collapse834e3(Checked 25.09.23)
Useful information for supporting children
UNICEF has information on talking to your child about COVID-19 here: https://www.unicef.org.au/blog/resources/march-2020/how-to-talk-to-your-children-about-coronavirus?dm_i=4W2U,BAIH,1FV16H,18L55,1 (Checked 25.09.23)
Childline has information here: https://www.childline.org.uk/info-advice/your-feelings/anxiety-stress-panic/worries-about-the-world/coronavirus/ (Checked 25.09.23)
The Association for Child Mental Health has released a podcast discussing the coronavirus and children and young people’s mental health. Read the news story and listen to the podcast: https://player.fm/series/association-for-child-and-adolescent-mental-health-acamh/dr-jon-goldin-on-the-coronavirus-and-child-mental-health (Checked 25.09.23)
Information about online safety
https://www.nspcc.org.uk/keeping-children-safe/online-safety/ (Checked 25.09.23)
If you express milk at work and are concerned about the possibility of contamination with COVID-19 the following information may help. This information was complied with healthcare workers in mind, but is relevant to anyone expressing milk at work.
The priority is your own safety, and that of your baby. If you are a healthcare worker caring for patients with COVID-19 while expressing for your own baby, the intensity of the environment may make fitting in these sessions harder.
No evidence has been found for COVID-19 being transmitted in breastmilk [1]. However, it has the potential to contaminate surfaces which could include the outside of bottles and breast pump. The following resources may be useful if you are working in an environment where this is a possibility e.g. patients have tested positive for COVID-19, or are suspected of having the virus.
The guide #COVID19 and Breastfeeding for Healthcare Professionals [2] is written by doctors for their own use. The guide covers practical options – handling your pump, and setting up a decontamination area at your front door. Good hand hygiene before and after expressing is vital along with careful cleaning of pump parts.
In the UK the general guidance for cleaning pumps and bottles is to follow the manufacturer’s instructions (RCOG / RCM Guidance [p78] below, [3]). General information on sterilising baby bottles can be found here: Sterilising baby bottles – NHS (www.nhs.uk) [4]
Milk storage containers are classed as a food contact surface and as such the use of chemical disinfectants on the outside of filled containers is not recommended (HMBANA, April 2020). [4] The HMBANA infographic guide [5] has suggestions for transferring milk after expressing into clean bottles which may be helpful. Standard milk storage times apply [6].
[1] Pietrasanta, C., Artieri, G., Ronchi, A., et al. (2022). SARS-CoV-2 infection and neonates: Evidence-based data after 18 months of the pandemic. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology, 33 Suppl 27, 96–98. https://doi.org/10.1111/pai.13643
[2] Breastfeeding and COVID-19 for HCPs (https://www.breastfeedingnetwork.org.uk/wp-content/uploads/2020/04/Breastfeeding-and-COVID-19-for-HCPs.pdf) (checked 31.08.22)
[3] Coronavirus (COVID-19) Infection in Pregnancy: Information for healthcare professionals Version 15: Published Thursday 7 March 2022 Coronavirus (COVID-19), infection in pregnancy | RCOG (checked 31.08.22)
[4] UK instructions for sterilising bottles and pump parts https://www.nhs.uk/conditions/pregnancy-and-baby/sterilising-bottles/ (checked 31.08.22)
[5] Milk Handling for COVID-19 Positive or Suspected Mothers in the Hospital Setting https://www.hmbana.org/news/milk-handling-for-covid-19-positive-or-suspected-mothers-in-the-hospital-setting.html (published 14.04.20, checked 31.08.22)
[6] Expressing and storing information https://www.breastfeedingnetwork.org.uk/breastfeeding-help/expressing-storing/ (checked 31.08.22)
Information on Breastfeeding support available during the COVID-19 pandemic is available here:
You can read a detailed summary of the research looking at the links between COVID-19 vaccines and fertility, pregnancy and breastfeeding, written by immunologist Dr Victoria Male, here: https://drive.google.com/file/d/1_wHIYX-tGkGBPwuax7N8BxZPR4PTTCDm/view
UK Health Security Agency information: https://www.gov.uk/government/publications/covid-19-vaccination-women-of-childbearing-age-currently-pregnant-planning-a-pregnancy-or-breastfeeding/covid-19-vaccination-a-guide-for-women-of-childbearing-age-pregnant-planning-a-pregnancy-or-breastfeeding (Updated 11.04.22, checked 31.08.22)
JCVI advises on COVID-19 vaccine for people aged under 40 https://www.gov.uk/government/news/jcvi-advises-on-covid-19-vaccine-for-people-aged-under-40 (published 07.05.21, checked 31.08.22)
Covid-19: UK offers under 40s alternative to AstraZeneca vaccine to boost confidence. British Medical Journal https://www.bmj.com/content/373/bmj.n1185 (published 10.05.21, checked 31.08.22)
NHS Coronavirus (COVID-19) vaccine information: who is eligible and which vaccine can they have: https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine/ (updated 21.07.22, checked 31.08.22)
Royal College of Obstetricians and Gynaecologists (RCOG) https://www.rcog.org.uk/guidance/coronavirus-covid-19-pregnancy-and-women-s-health/vaccination/covid-19-vaccines-pregnancy-and-breastfeeding-faqs/ (Updated 13.05.22, checked 31.08.22)
Public Health England : COVID-19 vaccination programme Information for healthcare practitioners https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/965177/COVID-19_vaccination_programme_guidance_for_healthcare_workers_26_February_2021_v3.4.pdf (Updated 09.03.22, checked 31.08.22)
GP Infant feeding Network (GPIFN) https://gpifn.org.uk/covid19/ (updated 11.06.21, checked 31.08.22)
Hospital Infant Feeding Network (HIFN) www.hifn.org/covid-interim (published January 2021, checked 31.08.22)
The UNICEF Baby Friendly Initiative information for healthcare professionals www.unicef.org.uk/babyfriendly/COVID-19/ (checked 13.04.22)
InfantRisk: https://www.infantrisk.com/covid-19-vaccine-pregnancy-and-breastfeeding?fbclid=IwAR030ND0pMXbF76x1zjCzj22HCrGGIUCirCFZ-ijHBFUBOeAECkVJQpMds0 (checked 31.08.22)
Academy of Breastfeeding Medicine: www.bfmed.org/abm-statement-considerations-for-covid-19-vaccination-in-lactation?fbclid=IwAR1qG7rS66IyTDyDlxGIOrwQsoSqDRuXWMWnjgBXwhOJuSofk13veeT3jl8 (published 14.12.20, checked 31.08.22)
The American College of Obstetricians and Gynaecologists: COVID-19 Vaccination Considerations for Obstetric–Gynecologic Care | ACOG (updated 05.08.22, checked 31.08.22)
The Green Book vaccination information for public health professionals: www.gov.uk/government/publications/covid-19-the-green-book-chapter-14a (updated 18.08.22, checked 31.08.22)
UNICEF Baby Friendly Initiative: https://www.unicef.org.uk/babyfriendly/COVID-19/ (checked 31.08.22)
Information from the World Health Organisation (WHO): https://www.who.int/health-topics/coronavirus#tab=tab_1 (checked 31.08.22)
The Royal College of Obstetricians and Gynaecologists have guidance for healthcare professionals caring for pregnant women and new mums here: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/covid-19-virus-infection-and-pregnancy/ (checked 31.08.22)
Bliss – for babies born premature or sick: https://www.bliss.org.uk/parents/support/coronavirus-covid-19-information (checked 31.08.22)
NHS Inform: pregnancy, breastfeeding and the coronavirus vaccine: Pregnancy, breastfeeding and the coronavirus vaccine | The coronavirus (COVID-19) vaccine (nhsinform.scot) (Checked 31.08.22)