Wendy Jones is BfN’s Pharmacist for our Drugs in Breastmilk Service. Here she talks about how we support mums with mental health issues, and points to some of the research, statistics, and useful resources about maternal mental health that inform her work.
 The Breastfeeding Network Drugs in Breastmilk Service has around ten thousand contacts with breastfeeding mothers annually. Some 20% of these queries relate to issues around mental health. We are passionate about supporting these mothers in accessing therapy and medication which enables them to continue to breastfeed if that is what they choose. As everyone who works within the service is a trained BfN helper or supporter we are also able to offer information on breastfeeding difficulties either on line, by using links or referring on to the National Breastfeeding Helpline.
The Breastfeeding Network Drugs in Breastmilk Service has around ten thousand contacts with breastfeeding mothers annually. Some 20% of these queries relate to issues around mental health. We are passionate about supporting these mothers in accessing therapy and medication which enables them to continue to breastfeed if that is what they choose. As everyone who works within the service is a trained BfN helper or supporter we are also able to offer information on breastfeeding difficulties either on line, by using links or referring on to the National Breastfeeding Helpline.
A survey monkey questionnaire we sent out last year showed that the dilemmas for mothers fell into several categories;
• Problems with breastfeeding was making the mother anxious or depressed
• Breastfeeding was a positive part of the mother’s relationship with her baby, but she needed medication to support her mental health issues
• Mothers for whom breastfeeding was going well but whose doctors or mental health team said that they couldn’t be prescribed medication unless they stopped breastfeeding
• Situations where mothers chose not to discuss their infant feeding with their professionals to avoid expected censure or debate, and where a drug had been prescribed with the doctor unaware that the mother was breastfeeding
• Mothers who were desperate not to take medication, but were struggling with mental health issues
• Decisions made the mother to stop breastfeeding to take medication

So many of us strive to be the perfect mum, reading lots of books, watching social media, running ourselves ragged to be at every group in order to give our children the best start. This not unsurprisingly leads to tiredness, depression and anxiety. It is something I remember doing 30 odd years ago with my babies. They must do Tumble Tots, must learn signing, must learn nursery rhymes leading to rhythm and pitch a precursor to music lessons, must learn to swim, must learn to share, must ………. Actually, what they remember now is being loved and happy. Some of the best times I spend with my grandbabies involves playing in the sand or sploshing in puddles etc.
Does social media add to the pressure and engender more depression and anxiety?
Our Drugs in Breastmilk service operates through Facebook. People can message me, and a team of other trained volunteers, and ask their medication and breastfeeding questions and we get back to them with an evidence based answer. However, the relationship between social media and mental health is a complex one. Professor Amy Brown, Associate Professor for Child Public Health at Swansea University, has shown some fascinating insights
- Conversation article, Social Media is Putting Pregnant Women Under Pressure to Look Perfect
- New Research Finds Link between some Baby Books and Post Natal Depression
Other research links Facebook use per se with depression
But social media can be a lifesaver in the middle of the night when you ask your trusted group for advice – or the opposite. Google searches can make you decide that you and/or your baby have some rare condition the outcome of which is terrible. Google (other search engines are available!) is not selective of evidence-based materials. If you look long enough you can find any viewpoint you want – it can reassure, and it can terrify.
Most of the contacts to the Drugs in Breastmilk service now come via social media – not just from the UK but across the world. We are continuing to develop fact sheets to answer the frequently asked questions. Nevertheless, many mums need reassurance that their personal situation is covered by the sheet be that in terms of dose, age of baby, other medications and we are happy to answer those questions. We also increasingly supply more in-depth information to healthcare professionals.
Relevant Statistics
Taken from “The costs of perinatal health problems”
• Between 10 and 20% of women develop a mental illness during pregnancy or within the first year after having a baby
• Perinatal depression, anxiety and psychosis carry a total long-term cost to society of about £8.1 billion for each one-year cohort of births in the UK.
• About half of all cases of perinatal depression and anxiety go undetected and many of those which are detected fail to receive evidence-based forms of treatment.
• Suicide is a leading cause of death for women during pregnancy and in the year after giving birth.
Prevalence of mental health conditions
• Antenatal depression; 7.4% in the 1st t trimester rising to14.8% in the 3rd trimester.
• Postnatal depression. 7.4 -11.0% in the first 3 months after childbirth, 7.8 – 12.8% in the 3rd to 6th months and 8.5 -12.0% in the 6th to 9th months
• Anxiety 11.8% – 15.3% during pregnancy and 8% in the period after birth
• Psychosis (refers to bipolar disorder, schizophrenia or very severe forms of depression). 0.2%. There are some developing studies that the condition may reach another peak following weaning (unpublished data reviewed)
• Obsessive Compulsive Disorder. 2.1% during pregnancy and 2.4% during the postnatal period compared with 1.1% in the general female population suggesting that pregnancy and giving birth might trigger the onset of the condition.
• Birth Trauma (Post Traumatic Stress Disorder (PTSD) that occurs after childbirth) 1.9-9% of births
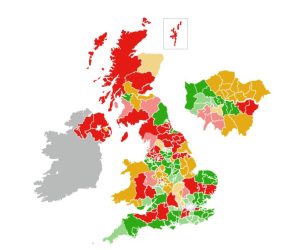
Provision of mental health services
Insights from mothers experiencing maternal mental health issues
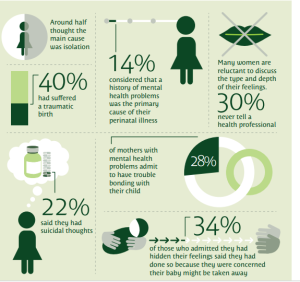
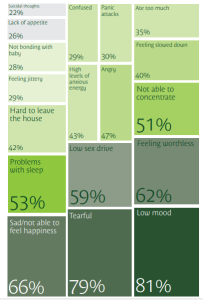
The Boots Family Trust wrote a fascinating report on Perinatal mental health experiences of women and health professionals 2013, which gives us some perspectives from the mothers themselves.
“How many of you have had a night out planned or arranged coffee with friends and suddenly the 4 walls you inhabit seem the only haven because it’s the only place you don’t have to pretend you are ok, so you cancel. Or when you are invited out you tell them how terribly sorry you are, but you’re already booked up that weekend, when you are actually just really busy holding it together in your safe box. And so, the first problem starts, all by itself. People stop asking you and the isolation that at first wasn’t true becomes your only truth”.
Several people who the outside world would see as confident and outgoing readily identified with the statement. Feeling socially anxious or in a place where you don’t want to go out is normal – let’s not stigmatise the feeling.
Mindfulness may help
Just before Christmas I was whiling away half an hour before catching a train, in a bookstore on Waterloo station. I bought a copy of “Frazzled” by Ruby Wax and devoured its contents. She felt like she was in my brain and understood ME. She is so honest about the stresses of life that crowd into our head – the buzzing in the brain which never ceases.
Tonight, I was listening to a radio 4 podcast by her and another lightbulb moment for me. “I wake up at 3 in the morning” she said, “and start doing emails frenetically, when I run out I check the spam box just in case then press refresh!” Oh, that is so what I do! She went on to say it is ok to rest, to watch a blackbird in the garden, to read poetry, to just be in the moment. I am currently trying to learn and practice the skill of mindfulness regularly. To be present in the moment, not the one which has just passed, not the one to come but just to be present at that instant. To accept thoughts but let them pass and not dwell on them.
This is a technique being more and more widely advocated for depression and anxiety. It isn’t easy as a mother to have as the wonderful story book my children loved “Five Minutes Peace” but just one minute can be enough to calm the brain, lower the adrenaline, stop the panic. I posted this guided mindfulness exercise on my own Facebook page recently which maybe some of you may find helpful. Keep going, don’t judge yourself, it isn’t a test it’s just being Mindful.
I have no financial link with any of these resources but have used and valued them myself.
Mental health and breastfeeding
Perinatal mental health issues affect many mothers. Some issues are caused by breastfeeding difficulties – the solution is to make more evidence-based, well-informed breastfeeding support available or to help mothers come to terms with why breastfeeding may not be for them in a positive, mother-centred, empathetic manner. Some issues need medical interventions which can be used during breastfeeding if the mother so wishes. Support of breastfeeding to the age of 2 years and beyond by all health professionals should be implicit. This is unlikely until breastfeeding is covered as a health promotion intervention in all undergraduate courses.
Mothers need to be listened to and their choices valued – whether that be in infant feeding choice or use of medication. Every one of us is an individual – that is what makes the human race so special, we are diverse and special.
What does the Breastfeeding Network do to support mothers with mental health issues in May 2018?
1. We have Drugs in Breastmilk fact sheets specifically written about:
• depression
• anxiety
• OCD
2. We provide additional information via social media and emails about the drugs used for mental health disorders
3. We are working with other organisations to support perinatal mental health
4. We are looking at how peer breastfeeding supporters can signpost to information on mental health
5. I deliver presentations to peer supporters and professionals normalising mental health conditions and looking at the safety of the drugs used to treat these conditions during breastfeeding
6. We are always striving to make links with other organisations supporting mothers and to work with them
7. We have made links with fathers who have mental health issues after the birth of their children
This was a comment on social media recently which I hope is exactly what I strive to do “Thank you so much. You provide a wonderful service and so much more than just drug knowledge “
Maternal Mental Health Matters Awareness Week 30th April – 6th May 2018
I will be fully engaged with Maternal Mental Health Matters Awareness Week 30th April – 6th May 2018
Tuesday 1 May Facebook Live session 7.30 pm Perinatal Mental Health Partnership
Friday 4th May Facebook live session from Mama Conference Glasgow, where BfN have been nominated as breastfeeding champions and I have been nominated as individual breastfeeding champion

